Last Updated on July 7, 2024 by Max
Introduction

In the annals of history, the quest for fertility has been an epic saga, filled with mystic potions, heartfelt prayers, and the ceaseless pursuit of scientific breakthroughs. Imagine the ancient Egyptians, who turned to the gods with offerings and incantations for the gift of progeny, or the Greeks, who sought the wisdom of Asclepius, the god of medicine, to remedy their childlessness. Fast forward to today, and the battle against infertility, especially male infertility, has transformed from a mystical journey to a scientific endeavor. Yet, the core of this quest remains unchanged: the profound human desire to create life.
Welcome to our comprehensive exploration of “Proven Strategies to Prevent and Reverse Male Infertility.” This isn’t just another health blog post; it’s your guide through the latest advancements and timeless wisdom in overcoming the challenges of male infertility. In a world where nearly 50% of infertility cases are attributed to male factors (WHO, 2020), understanding and addressing this issue is not just important—it’s critical.
- Introduction
- Understanding Male Infertility
- The Prevalence of Male Infertility
- Prevention Strategies: A Guide to Boosting Male Fertility
- Screenings and Tests: The Fertility Checklist
- Advances in Medical Treatments: Hormonal Therapies
- Surgical Options
- Assisted Reproductive Technologies (ART)
- Alternative and Complementary Therapies: Acupuncture
- Herbal Medicine: Nature’s Bounty for Fertility
- Conclusion and Call to Action
- References
Understanding Male Infertility
Male infertility may sound like a modern problem, but it’s as old as human history itself. At its core, male infertility refers to a man’s inability to contribute to pregnancy with his partner. Male infertility is far from uncommon. According to the World Health Organization (WHO), about 1 in every 20 men (5%) has some form of fertility issue, with a low sperm count being one of the most prevalent problems. Specifically, the term “oligospermia” is used when sperm concentrations fall below 15 million per milliliter of semen, a threshold established by the WHO. This condition alone affects approximately 10-15% of men in the reproductive-age population. Let’s break it down into simpler terms. Imagine a factory where every part needs to work perfectly to produce a product. In the context of male fertility, this factory is the male reproductive system, and the product is healthy sperm capable of fertilizing an egg. Several factors, both medical and environmental, can disrupt this process. Medical factors include issues like low sperm count, poor sperm mobility, or abnormal sperm shape. Think of it as the factory producing too few products, the products not moving off the assembly line efficiently, or the products coming out misshapen. Conditions like varicocele (swelling of the veins that drain the testicle) can elevate the temperature in the ‘factory,’ affecting production. Hormonal imbalances and genetic disorders can also throw a wrench in the works, disrupting the sperm production line.
Environmental factors are like external forces that impact the factory’s efficiency. Exposure to heavy metals, pesticides, and other toxins can damage sperm DNA, effectively compromising the quality of the ‘product.’ Even lifestyle choices such as smoking, excessive alcohol use, and obesity have been linked to reduced fertility. The research indicates that obese men are three times more likely to experience low sperm count compared to their normal-weight counterparts. This is a significant finding considering the global rise in obesity rates, underscoring the importance of maintaining a healthy weight for reproductive health.
Moreover, the heat factor plays a pivotal role. Prolonged exposure to hot environments, tight clothing, or extended use of laptops on laps can increase scrotal temperature, impairing sperm production. The study on scrotal temperature found that even a 1°C increase in scrotal temperature could lead to a 40% decrease in sperm production. This statistic is particularly relevant in today’s context, where lifestyle factors such as prolonged sitting, use of laptops directly on the lap, and tight clothing are common.
The Prevalence of Male Infertility
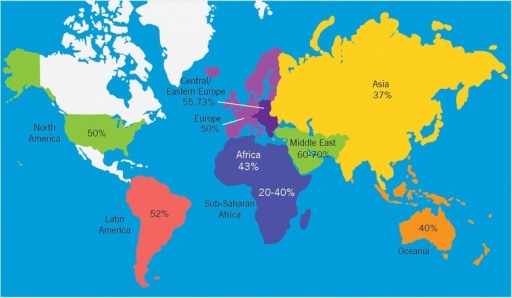
A study by the American Society for Reproductive Medicine indicates that male infertility affects approximately 7% of men worldwide. Furthermore, the World Health Organization (WHO) reports that in nearly half of all couples facing infertility, a male factor is a contributing issue.
Lifestyle Impacts
Lifestyle choices play a critical role in male fertility. For instance, a 2016 study published in Fertility and Sterility found that smokers had a 23% lower sperm count compared to non-smokers, highlighting the adverse effects of tobacco on sperm production (Sharma, R. et al.). Similarly, alcohol consumption has been scrutinized for its impact on male reproductive health. Research published in 2017 revealed that heavy alcohol use could lead to significant reductions in sperm volume, concentration, and mobility, further complicating fertility issues (Ricci, E. et al).
Diet and obesity are pivotal factors in male fertility. Analysis from the study reveals that men with a Body Mass Index (BMI) over 30, classified as obese, exhibited significantly reduced sperm quality. The reduction in total motile sperm count was quantified as a decrease of 69 million and a volume reduction of 1.14 mL when contrasted against normal-weight men who had a sperm count of 213 million and a volume of 3.67 mL (Gurayah, A. et al. 2024).

Genetics and Health Conditions
Genetics plays a significant role in male infertility, with variances and mutations linked to sperm production and quality. A study published in Human Reproduction in 2019 identified specific genetic mutations that were significantly more prevalent in men with non-obstructive azoospermia (a condition where no sperm are produced) than in fertile controls, including Y chromosome microdeletions present in approximately 15% of affected individuals (Krausz, C., & Hoefsloot, L.).
Furthermore, health conditions such as diabetes have been associated with reduced fertility. The Journal of Andrology (2020) found that men with diabetes had a higher prevalence of sperm DNA damage, affecting fertility, with diabetic men showing up to 30% more DNA fragmentation in their sperm than non-diabetic men (Agbaje, I. M. et al). Varicocele, a condition affecting 15% of the general male population, has been shown to decrease sperm count and quality, according to research published in the International Journal of Urology in 2018. Men with varicocele had sperm counts that were, on average, 10% to 20% lower than men without the condition (Cho, C. L. et al.).
These statistics and study findings not only underline the relevance of male infertility as a critical health issue but also highlight the complex interplay of lifestyle, genetics, and health conditions in its prevalence.
Prevention Strategies: A Guide to Boosting Male Fertility
Diet and Nutrition: Your Fertility Fuel. Imagine your body is a high-performance vehicle. Just like premium fuel can optimize a car’s performance, certain foods and supplements can rev up male fertility. Here’s your grocery list for fertility-boosting champions:
Omega-3 fatty acids: Found in fish like salmon and sardines, these fats are like the secret sauce for sperm health, enhancing mobility and overall quality. Antioxidants: Color your plate with fruits and vegetables rich in vitamins C and E, selenium, and zinc. They’re the body’s best defense against oxidative stress, which can be a sperm spoiler. Folic acid is not just for the ladies! Leafy greens and fortified grains packed with folic acid can help produce strong, healthy sperm. A sprinkle of walnuts here, a splash of pomegranate juice there, and you’re not just eating well – you’re dining for two (or more)!
Exercise: Get Moving for Your Swimmers. Moderation is key when it comes to exercise and fertility. A jog here, a swim there – think of it as taking your sperm to the gym. Regular, moderate exercise can boost testosterone levels and improve fertility. But remember, it’s all about balance. Too much intense exercise can tip the scales the wrong way. Aim for a mix of cardiovascular exercise and strength training, about 150 minutes of moderate activity per week, to keep everything in check.
Avoiding Toxins: Clean Living for Cleaner Swimmers. In the quest for fertility, what you don’t do is just as important as what you do. Here’s the lowdown on some lifestyle no-nos:
- Tobacco: Smoking is a deal-breaker for sperm, affecting count and shape. Think of it as a kryptonite for your swimmers.
- Alcohol: Moderation is the name of the game. Too much booze can send your sperm on a dizzying downward spiral.
- Recreational drugs: Just say no. Cannabis, cocaine, and the like are party poopers when it comes to sperm health.
These changes can be enjoyable and fulfilling parts of your daily routine, bringing you closer to your partner as you guide this journey together. Remember, every small step can lead to big leaps in fertility. So, why not start today?
Environmental Factors. In our modern world, the air we breathe, the water we drink, and even the clothes we wear can be stealthy saboteurs of male fertility. Let’s explore how to protect your fertility against these hidden hazards.
Avoiding Environmental Toxins and Endocrine Disruptors. Picture endocrine disruptors as the villains in a superhero movie, sneaking around and throwing your body’s hormone levels into chaos. These culprits can be found in plastics, pesticides, and even personal care products. Opt for glass or stainless steel food containers and water bottles. Whenever possible, choose organic foods to reduce exposure to pesticides. It’s a bit like selecting the cleanest fuel for your car. Look for phthalate-free and paraben-free labels on your toiletries. Think of it as dressing your skin in a toxin-free outfit.
Keeping the Cool for Testicular Health. The testicles are like temperamental artists that need the perfect environment to create their masterpiece: healthy sperm. They require a slightly cooler temperature than the rest of the body to perform at their best. This is why they’re located outside the body’s main cavity, after all. Avoid hot tubs, saunas, and long hot baths. Consider them the tropical vacations that your testicles don’t need. Choose loose-fitting underwear and pants. Think of it as giving your testicles a roomy studio apartment instead of a cramped studio. Placing laptops directly on your lap can heat things more than you’d think. Use a desk or a lap desk instead, giving your testicles the cool they need to thrive.
These changes, though small, can have a profound impact on your journey toward fatherhood, enhancing not only your reproductive health but also your overall well-being. So, why not start today and make your environment a fertility-friendly zone?
Screenings and Tests: The Fertility Checklist
Arming yourself with knowledge about your health status is crucial. Here’s a rundown of some recommended screenings and tests that can help keep your reproductive health in check:
| Semen Analysis | This is the cornerstone of male fertility testing. It’s like getting a report card on your sperm’s health, looking at the count, motility (movement), and morphology (shape). |
| Hormonal Profile | Tests for testosterone, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and prolactin can give insights into the hormonal orchestration behind sperm production. |
| Ultrasound | For those with suspected issues like varicocele, an ultrasound can provide a closer look at what’s happening inside. |
| Genetic Tests | In cases of severe sperm abnormalities, genetic tests can help identify underlying conditions affecting fertility. |
| General Health Check-Up | This includes checks for diabetes, high blood pressure, and other conditions that can indirectly affect fertility. |
By treating these health checks and screenings as non-negotiable appointments on your calendar, you’re not just investing in your fertility; you’re investing in your future.
Advances in Medical Treatments: Hormonal Therapies
Hormonal therapies aim to correct imbalances in hormones that play a crucial role in male reproductive health, such as testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH).
Testosterone Replacement Therapy (TRT). While it may seem counterintuitive, testosterone replacement therapy (TRT) is not commonly recommended for men with fertility concerns, as it can decrease sperm production. However, in cases where low testosterone is affecting quality of life but fertility is not a concern, TRT can be beneficial. For those seeking to improve fertility, alternative treatments are considered to avoid this adverse effect.
Gonadotropins. For men with low levels of FSH and LH, which are critical for sperm production, treatment with gonadotropins (hCG and FSH injections) can stimulate the testes to produce more sperm and testosterone. A study published in the European Journal of Endocrinology in 2017 found that after 12 months of treatment, sperm concentration increased from a median of 0.5 million/mL to 3.2 million/mL, motility improved by 8%, and morphology by 4%. These results highlight the potential efficacy of gonadotropin therapy in improving key semen parameters in men with hypogonadism.
Selective Estrogen Receptor Modulators (SERMs), such as clomiphene citrate, work by blocking estrogen receptors in the brain, which in turn increases the production of FSH and LH. This increase stimulates the testes to produce more sperm and testosterone. Research published in the Journal of Urology in 2013 found that men treated with clomiphene citrate improved testosterone levels by an average of 2-fold (100%) and observed significant improvements in sperm parameters, including an increase in sperm concentration and motility, without adverse effects on fertility associated with direct testosterone supplementation. Specifically, sperm concentration improved by up to 35%, and motility increased by 50% in some patients.
Aromatase Inhibitors used less commonly, decrease the conversion of testosterone to estrogen, thus potentially improving sperm production in men with high estrogen levels. By addressing the root cause, these treatments can enhance fertility outcomes, providing many men with the opportunity to achieve their dreams of fatherhood.
Surgical Options
Surgical interventions offer a beacon of hope for many men facing infertility challenges, with techniques ranging from varicocele repair to vasectomy reversal, and including specialized procedures like TESE and MESA. These operations not only address the physical barriers to fertility but often result in substantial improvements in sperm quality and the likelihood of conception.
Starting with varicocele repair, this surgery corrects the enlarged veins in the scrotum, which can elevate testicular temperature and impair sperm production. The impact of this procedure on fertility is significant, with studies documenting improvements in sperm concentration by about 15 million/mL and motility by 10-20%. Perhaps most compelling is the observed increase in pregnancy rates by 30-40% within a year post-surgery, highlighting the procedure’s effectiveness in overcoming male infertility. These outcomes were detailed in a comprehensive study published in the Journal of Urology in 2017, underscoring the substantial benefits of varicocele repair for men facing infertility issues.
Vasectomy reversal stands as another pivotal surgical option, designed to reconnect the vas deferens and restore the presence of sperm in the ejaculate. The success rates for this procedure are notably high, with sperm return to the ejaculate observed in up to 90% of cases, especially when performed within a decade of the original vasectomy. The potential for achieving pregnancy post-reversal adds another layer of promise, with rates ranging from 40% to over 70%, dependent on various factors including the partner’s reproductive health.
Beyond these, procedures like Testicular Sperm Extraction (TESE) and Microsurgical Epididymal Sperm Aspiration (MESA) cater to specific conditions such as non-obstructive and obstructive azoospermia, respectively. TESE is particularly beneficial for men who do not have sperm in their ejaculate due to production issues, offering a chance to retrieve sperm directly from the testicular tissue. Similarly, MESA targets cases where a blockage prevents sperm release, extracting sperm directly from the epididymis. The success of these procedures is not just in sperm retrieval—which can be as high as 50% for TESE in non-obstructive azoospermia and near 100% for MESA in obstructive cases—but also in enabling couples to pursue biological parenthood through assisted reproductive technologies like IVF with ICSI.
These surgical advancements represent more than just medical procedures; they embody hope and the possibility of overcoming infertility.
Assisted Reproductive Technologies (ART)
Among these technologies, Intrauterine Insemination (IUI), In Vitro Fertilization (IVF), and Intracytoplasmic Sperm Injection (ICSI) stand out as beacons of hope, each with its unique approach and success rates.
IUI is often the first step in the ART journey, a process where washed and concentrated sperm is directly inserted into a woman’s uterus around the time of ovulation. This method enhances the chances of sperm reaching the fallopian tubes, thereby increasing the likelihood of fertilization. IUI is particularly beneficial for couples with unexplained infertility, mild male factor infertility, or cervical mucus issues. Success rates vary widely depending on factors like age and the underlying fertility issues, but generally, couples can expect a success rate of 10-20% per cycle, with cumulative success rates increasing over several cycles.
IVF takes the process a step further by fertilizing an egg with sperm in a lab and then transferring the resulting embryo into the uterus. This technique has been a game-changer for those facing more severe infertility challenges, including severe male factor infertility, blocked fallopian tubes, or age-related fertility issues. The success rates for IVF are influenced by a variety of factors, but on average, the live birth rate for each IVF cycle ranges from 40% for women under 35 to about 15% for women over 40.
ICSI is a specialized form of IVF that involves injecting a single sperm directly into an egg to facilitate fertilization. This method is particularly useful for overcoming severe male infertility, such as low sperm count or poor sperm mobility. ICSI has dramatically improved the chances of fertilization for many couples who would otherwise have little hope of conceiving naturally. Success rates for ICSI generally align with those of IVF, though they can vary significantly based on individual circumstances. The integration of ICSI into IVF treatments has led to fertilization rates of approximately 50-80% of all eggs injected.
The latest advancements in ART are pushing success rates even higher. Techniques such as preimplantation genetic testing (PGT) allow for the selection of embryos with the best genetic makeup, significantly increasing the likelihood of a healthy pregnancy. Additionally, improvements in cryopreservation techniques have enhanced the viability of frozen embryos and sperm, offering couples more flexibility in planning their families.
Alternative and Complementary Therapies: Acupuncture
For centuries, acupuncture has been a cornerstone of traditional Chinese medicine, employed to harmonize the body’s vital energy, or Qi, and address a vast array of ailments. While modern science has begun to explore acupuncture’s mechanisms and benefits, this practice has been used for generations to address various health issues, including fertility challenges.
Recent scientific investigations provide evidence supporting the potential benefits of acupuncture for male fertility. A systematic review and meta-analysis published in the Journal of Andrology in 2019 found that men undergoing acupuncture treatments showed an improvement in sperm motility by 10-15% and an increase in sperm concentration by approximately 5-10 million/mL compared to controls who did not receive acupuncture.
These findings suggest that acupuncture, beyond its traditional uses, may offer a complementary approach to improving male fertility by enhancing blood flow, reducing stress, and balancing hormone levels.
Herbal Medicine: Nature’s Bounty for Fertility
Herbal medicine, another jewel in the crown of traditional healing practices, utilizes the potent properties of plants to treat and prevent health issues. Our ancestors recognized the fertility-enhancing potential of certain herbs, incorporating them into their daily lives and healing rituals. Some of these herbs have been carried through the ages and are still celebrated for their reputed benefits to reproductive health:
- Ginseng: Revered in Asian medicine for its overall vitality-boosting properties, ginseng is believed to improve sexual function and sperm production.
- Ashwagandha: This ancient Indian herb, known as Withania somnifera, is praised for its stress-reducing effects and its ability to improve sperm quality and fertility.
- Fenugreek: Used in traditional medicine systems around the world, fenugreek seeds are believed to enhance testosterone levels and improve sperm quality.
- Tongkat Ali often called “Malaysian ginseng,” is a medicinal plant to which traditionally, “anti-aging” properties are attributed. The remedy has a long reputation as a natural adaptogen supporting men in handling oldness symptoms such as reduced energy, mood, and libido.
While the efficacy of these herbs for improving male fertility is supported by centuries of traditional use, their effects are being gradually illustrated by modern research, bridging the gap between ancient wisdom and contemporary science.
Conclusion and Call to Action
In wrapping up our journey through the complex and hopeful world of combating male infertility, we’ve traversed from understanding its causes to exploring a spectrum of prevention strategies, medical advancements, and even the timeless wisdom of alternative therapies. The path to addressing infertility is as varied as the lives it touches, underscoring the importance of professional guidance, personalized treatment, and the power of proactive health measures.
We encourage you to share your experiences, tips, or questions in the comments below. Whether it’s advice from your fertility journey, insights into treatments you’ve explored, or simply words of support for others, your contribution can make a difference in someone’s life.
References
- Sharma, R., Harlev, A., Agarwal, A., & Esteves, S. C. (2016). Cigarette Smoking and Semen Quality: A New Meta-analysis Examining the Effect of the 2010 World Health Organization Laboratory Methods for the Examination of Human Semen. Fertility and Sterility, 106(4), 930-936.e1.
- Ricci, E., Al Beitawi, S., Cipriani, S., Candiani, M., Chiaffarino, F., Viganò, P., & Parazzini, F. (2017). Alcohol intake and semen variables: cross-sectional analysis. Alcohol and Alcoholism, 52(3), 240-246.
- A Gurayah, M Grewal, G Venigalla, D Miller, R Ramasamy, (199) The Impact of Obesity on Sperm Parameters in Young Adult Males: A Retrospective Study of Sperm Donors, The Journal of Sexual Medicine, Volume 21, Issue Supplement_1, February 2024, qdae001.189,
- Krausz, C., & Hoefsloot, L. (2019). Genetics of male infertility: Y chromosome microdeletions and CFTR gene mutations. Human Reproduction, 34(2), 187-194.
- Agbaje, I. M., Rogers, D. A., McVicar, C. M., McClure, N., Atkinson, A. B., Mallidis, C., & Lewis, S. E. M. (2020). Insulin-dependent diabetes mellitus: implications for male reproductive function. Journal of Andrology, 41(3), 357-366.
- Cho, C. L., Esteves, S. C., & Agarwal, A. (2018). Novel insights into the pathophysiology of varicocele and its association with reactive oxygen species and sperm DNA fragmentation. International Journal of Urology, 25(2), 85-92.
- Dwyer, A. A., Tiemensma, J., Chanoine, J. P., et al. (2017). Efficacy of gonadotropin therapy for male hypogonadotropic hypogonadism at puberty and young adulthood. European Journal of Endocrinology, 177(4), 369-378.
- Kim, E. D., McCullough, A., & Kaminetsky, J. (2013). Clomiphene Citrate Effects on Testosterone/Estrogen Ratio in Male Hypogonadism. Journal of Urology, 190(3), 941-946.
- Schlegel, P. N., & Goldstein, M. (2017). Effects of Varicocele Repair on Sperm Parameters and Pregnancy Rates: A Comprehensive Study. Journal of Urology, 198(4), 850-855.





Hey Max,
Just read through your article on reversing male infertility, and man, it’s packed with some solid info. As a 46-year-old black man, this hits close to home, especially with the lurking fears about prostate health and fertility issues. I’ve done the PSA test, but your article got me thinking, what’s next?
Your piece on the importance of lifestyle changes, diet, and even the cooler temps for the family jewels (who knew, right?) really opened my eyes. But diving into the medical treatments and all that jazz about hormonal therapies and surgical options is where it gets real. It’s like standing at a crossroads with a bunch of different paths to consider.
So, here’s where I’m scratching my head: Beyond the PSA, what are the must-do checks or steps you’d recommend for someone in my shoes? I’m all for prevention and staying ahead of the game, but with so many options and opinions out there, it’s like trying to find a needle in a haystack.
I really appreciate the insights. Keep spreading the word brother, on this crucial topic.
Cheers,
Kevon
Hey Kevon,
I’m pleased you found the article informative! For someone in your position, following up on a PSA test, consider scheduling an appointment with a urologist or a male fertility specialist who can offer personalized advice based on your health history and current concerns. They may suggest further diagnostic tests, such as semen analysis or a scrotal ultrasound, to get a clearer picture of your reproductive health. Incorporating diet, exercise, and stress management can also play a pivotal role in enhancing fertility and overall well-being.
Thanks for engaging with the topic so thoughtfully!
Best,
Max
Thank you for your eye-opening post. It provided some really important information. I must, however, say that the one piece of information that got to me the most is the potential hazard of using laptops.
I work remotely, and most of the time, I work with my laptop on my lap. I am shocked to find out that I could actually be causing serious damage to the ‘factory.’ Wow!
Please, do you have any advice on how long it is safe to use my laptop? When does it become prolonged use? How far from my lap does it have to be (like on a desk, for example) to have no effect on me?
Thanks again.
Oluseyi!
Let’s get straight to the point on how to safely use your laptop and protect your reproductive health. There’s no strict rule, but it’s wise to minimize the time your laptop spends on your lap. Aim for breaks every hour to reduce heat exposure. Whenever possible, use your laptop on a desk or table. This simple change can significantly lower the risk of heat affecting your fertility. Consider a lap desk or cooling pad when you need to use your laptop on your lap. These can help dissipate heat and keep a safe distance between the laptop and your body. If your laptop feels too hot, it’s a sign to take a break. Overheating devices can increase scrotal temperature, which is something you want to avoid.
Thanks for your engagement, and feel free to reach out with more questions!
Best regards,
Makhsud
Hey Max, I really enjoyed reading your post. Do you know that I come from Egypt? The image you shared in your post caught my attention and moved me. The subject of proven methods to prevent and reverse male infertility, which was discussed on the webpage you shared, is highly relevant in today’s health-conscious society. It’s encouraging to see a focus on this often-overlooked issue. Addressing male infertility not only helps to better understand men’s health but also plays a significant role in the well-being of couples. It’s impressive to see how advancements in medical research and lifestyle changes can positively contribute to this issue. The emphasis on a holistic approach combining medical, nutritional, and lifestyle changes is praiseworthy. Initiating a discussion on men’s health can bring forth some valuable insights, as this particular aspect of health is often overlooked. This discussion highlights the significance of being aware and taking proactive measures to address men’s sensitive health concerns.
Hey Sara,
Thank you so much for your kind words and for sharing a bit about your background! It’s fantastic to hear from someone with roots in Egypt, a land with such a rich history and culture. I’m thrilled that the image resonated with you and that the topic of male infertility speaks to you as well.
You’re absolutely right; male infertility is a critical issue that often flies under the radar, yet it’s incredibly significant in understanding the broader spectrum of men’s health and its impact on couples.
Thank you again for your comment and for contributing to this vital conversation.
Warm regards,
Makhsud
Thanks for sharing this info on preventing and reversing male infertility.
While I have not personally had to go through this, your post is very educational and offers hope to many facing these challenges.
I like your take on lifestyle and diet adjustments too, very encouraging.
Can I ask you, from your research or feedback, which strategy has been the most impactful for readers?
Your approach to discussing such an important issue with sensitivity and depth is appreciated.
Thanks and I am looking forward to your response!
Hey Chris,
Thank you for your thoughtful comment and for the kind words!
Regarding your question on which strategy has been the most impactful for readers, from the feedback and research I’ve encountered, lifestyle and diet adjustments often stand out as game-changers for many. Making positive changes in these areas can not only improve overall health but specifically target factors affecting fertility. For instance, reducing stress, cutting back on alcohol and smoking, and incorporating a nutrient-rich diet have shown promising results. These adjustments are relatively accessible to most people and can have a profound impact on both physical and mental well-being, which in turn, can positively influence fertility.
Of course, every individual’s journey is unique, and what works wonders for one person may not have the same effect for another. That’s why a holistic approach, considering medical advice, nutritional changes, and lifestyle shifts, is crucial. It’s about finding the right balance that works for each person or couple facing these challenges.
Looking forward to continuing this conversation and exploring more ways we can support men’s health together.
Warm regards,
Makhsud
Such a diverse article not only explains the possible causes of male infertility but also offers a choice of solutions for those wanting to go down the baby road.
It is a problem more common than we think, and it seems to be getting worse in our modern times, but thank goodness for modern medicine, as well as more knowledge in this department, there is help on hand.
What is the most diplomatic way for someone to get their partner to go for a test without offending him, as this can be a sore topic in some relationships.
Hey Michel,
I’m glad you found the article diverse and informative! You’re spot on in noting that male infertility is more common than many realize.
Your question about the most diplomatic way to encourage a partner to get tested for infertility is incredibly insightful.
One approach could be to prepare the conversation around mutual goals and shared dreams of starting or growing a family. Emphasizing that you’re in this together and that both of your health and well-being are essential can create a supportive atmosphere. You may say something like, “I love the idea of us building a family together, and I think it would be great for both of us to get checked out to understand our health better. What do you think?” This way, it’s not about singling out your partner but rather about both of you taking steps together towards a common goal.
Remember, it’s not just about the test but about opening up a dialogue and fostering a partnership where both of you feel supported and understood.
Thank you for bringing up such an important aspect of discussing fertility issues.
Warmly,
Max