Last Updated on July 7, 2024 by Max
Introduction
Erectile dysfunction (ED) is a common health issue affecting men’s lives, relationships, and well-being. One potential contributor to this condition is varicocele—a swelling in the veins that drain the testicle. However, not an absolute cure for ED; addressing a varicocele could form an integral part of a comprehensive approach to managing the symptoms of ED. In this article, we delve into the relationship between varicocele and ED, shedding light on how treatment might facilitate the latter.
The Scope of Erectile Dysfunction
ED is a condition marked by persistent difficulty achieving and maintaining an erection sufficient for satisfactory sexual performance. This widespread medical issue affects approximately 52% of men between 40 and 70 years old, according to a report by the Massachusetts Male Aging Study (Feldman et al., 1994). Alarmingly, one in four patients seeking medical help is under 40, with half suffering from severe ED.
Understanding the Connection Between ED and Varicocele
ED often co-occurs with cardiovascular diseases, sharing several risk factors such as obesity, abnormal lipid levels, diabetes, lack of exercise, and smoking. This correlation stems from the complex interplay between our nervous, hormonal, and cardiovascular systems needed for an erection.
A varicocele, on the other hand, is a form of venous insufficiency affecting the testicular veins. This condition can impede the outflow of waste materials and testosterone from the testes, thereby impacting their functionality. A varicocele can thus influence two vital components of a man’s reproductive system:
- Prostate: A varicocele can stimulate an overgrowth of the prostate, causing benign prostatic hyperplasia and leaving the gland susceptible to inflammation and bacterial infections (prostatitis), both of which can affect penile erection.
- Testicles: A varicocele disrupts the normal process of sperm production and testosterone secretion, which can lead to decreased sexual desire.
The Impact of Varicocele on ED
In a comprehensive study involving 32,856 cases and 98,568 controls, Keller and colleagues (2012) discovered a significant correlation between varicocele, its surgical treatment (varicocelectomy), and ED. They found that varicocele patients who underwent surgery had lower risks of developing ED compared to untreated patients. Furthermore, they observed the strongest association between varicocele and ED in the youngest men.
Varicocele, Low Testosterone, and Sexual Health
ED, low testosterone, infertility, and hypogonadism are interrelated conditions. This relationship becomes apparent when we consider that premature ejaculation and decreased sexual desire are commonly reported in men with varicocele and infertility. Additionally, low blood testosterone levels caused by varicocele are linked to reduced libido.
Testosterone, the primary male hormone, is a crucial indicator of hypogonadism. While there’s no universally accepted lower limit of normal, a testosterone level below 350 ng/dl is typically a red flag for hypogonadism.
Numerous studies reported a strong association between varicocele and impaired testicular function. The three main types of cells in testicles are:
- Leydig cells, producing testosterone;
- Sertoli cells, nourishing and supporting sperm cells;
- Sperm cells themselves.
For the natural flow of events, the proliferation of sperm cells, and the production of testosterone, the temperature of the testicles must be somewhat lower than the body temperature. That’s why we have the testicles outside the body, in the scrotum.
Varicocele results in increased testicular temperature, harming spermatogenesis, impairing Sertoli cell function, depressed testosterone synthesis, and Leydig cells atrophy.
Studies have indicated that varicocele repair can increase testosterone levels, signifying improved testicular functionality (Dabaja & Goldstein, 2016). This improvement was observed regardless of the patient’s age, highlighting the benefits of varicocele treatment across different age groups. Summarised results of the relevant studies are presented in the table.
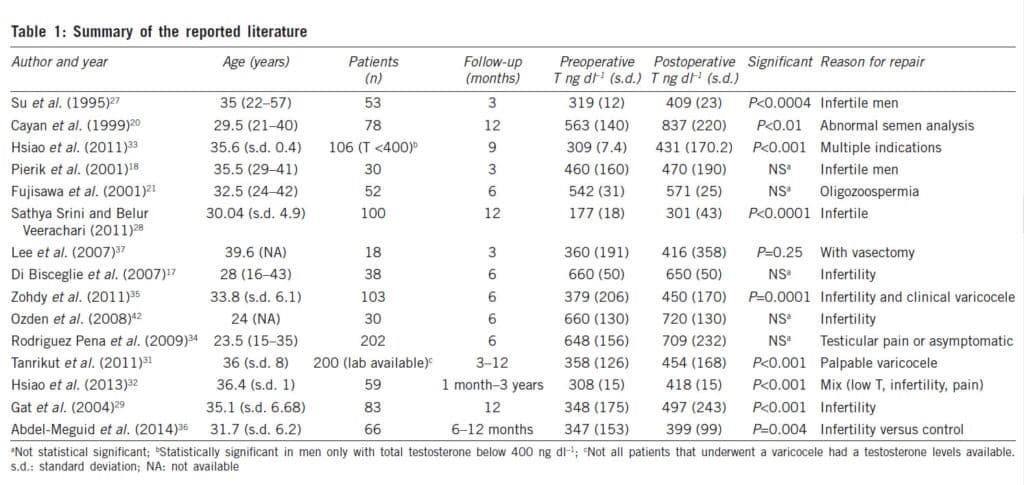
They suggest that varicocele repair improves testicular functionality: the blood testosterone level increases between 100 and 140 ng/dl in more than 80% of men. And what was interesting, the lower the testosterone levels before varicocele repair, the more significant its changes after the treatment were. Moreover, in adult men of 50-60s, the total testosterone improved as much as in younger men.
Conclusion: The Importance of Early Varicocele Treatment
While many men with varicoceles are fertile and do not exhibit ED symptoms, the growing body of evidence regarding the adverse effects of varicocele on fertility, premature ejaculation, testosterone levels, and ED should not be overlooked. Prevention is generally easier and more effective than treatment after the onset of these conditions. Early intervention and varicocele repair may prevent future fertility issues and hormonal imbalances.
In men with testosterone levels exceeding 300 ng/dl, varicocelectomy may not result in significant hormonal changes. However, such a procedure could safeguard testicular function and preclude future declines in testosterone levels.
We encourage health practitioners and patients to consider varicocele treatment as part of a comprehensive approach to managing ED symptoms. By addressing the underlying causes, we can improve outcomes and significantly enhance the quality of life for men dealing with ED.
Do you have any experiences or thoughts you’d like to share? We invite you to contribute to the discussion in the comments below.
References
- Feldman, H. A., Goldstein, I., Hatzichristou, D. G., Krane, R. J., & McKinlay, J. B. (1994). Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. Journal of urology, 151(1), 54-61.
- Keller, J. J., Chen, Y. K., & Lin, H. C. (2012). Varicocele is associated with erectile dysfunction: a population-based case-control study. The journal of sexual medicine, 9(6), 1745-1752.
- Dabaja, A. A., & Goldstein, M. (2016). When is a varicocele repair indicated: the dilemma of hypogonadism and erectile dysfunction? Asian journal of andrology, 18(2), 213–216.