Last Updated on July 7, 2024 by Max
Introduction
Until recently, the relationship between benign prostate hyperplasia (BPH) and prostate cancer (PC) remained controversial. Some studies have found such a relationship, while others, on the contrary, could not find any association between them. Therefore, the idea of the independence of these prostate conditions has been propagated to reduce the fear of most people suffering from BPH symptoms of a possible escalation into PC. The larger your prostate, the less your chance of getting prostate cancer – this is the main conclusion of the recent study by K. R. Nandalur et al.(2021).
The results of a recent study published in “The Prostate” not only resolve these inconsistencies but, most importantly, confirm a significant inverse relationship between prostate size and the risk of PC. In the post, we will discuss this study, the results of which others will hopefully confirm.
The main effects of the prostate enlargement
– Age-related prostate enlargement is a sign that your body protects your prostate from PC.– One cm3 increase in the central gland volume is associated with an approximately 3% decrease in risks for adverse prostate cancer.- Using 5-alfa reductase inhibitors to manage BPH symptoms leads to delayed diagnosis and worse cancer-specific outcomes in men with PC.
- Introduction
- Common Features and Differences Between Benign Prostate Hyperplasia and Prostate Cancer
- Is There an Association Between BPH and PC?
- The Larger the Central Gland, the Lower the Risk of Prostate Cancer
- Should We Reduce the Size of the Prostate to Alleviate the BPH Symptoms?
- Conclusions
- References
Quiz Time: Prostate Health Myths vs. Facts
Common Features and Differences Between Benign Prostate Hyperplasia and Prostate Cancer
Despite the seeming similarity of BPH and PC:
- They both are diseases of the prostate,
- Share low urinary tract symptoms, and
- Underlying mechanisms for both conditions often are linked to hormonal imbalances and inflammation,
They often occur in distinct anatomic regions, with BPH affecting the Central Gland (CG), composed of the Transitional Zone and Central Zone, and PC – in the Peripheral Zone (PZ).
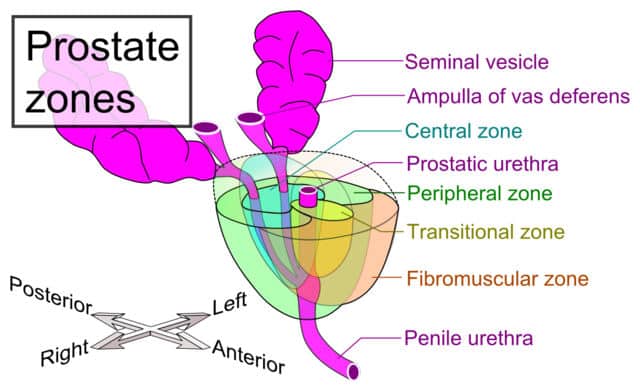
The Central Zone surrounds the ejaculatory ducts of the prostate and forms about 25% of its volume. About 5% of PC cases arise in this zone.
The Transitional Zone is the innermost part of the prostate surrounding the urethra, composing about 5% of the prostate gland. TZ grows throughout men’s lives. Cell proliferation in this zone and the central zone results in benign prostatic enlargement as men age over 50. About 10% of prostate cancers originate in this zone.
The Peripheral Zone is the outermost area of the prostate, found mainly in the back of the gland closest to the rectum. PZ forms about 70% of the prostate volume. About 80% of prostate carcinomas arise in the PZ.
Is There an Association Between BPH and PC?
The Prostate Cancer Prevention Trial (Schenk JM. et al., 2011 ) showed no association between PC and symptomatic BPH. The trial included 1,225 men whose cancer was detected and 3,843 men with a biopsy-proven PC absence. The conclusion of the trial was: “This study provides the most robust evidence to date that BPH does not increase the risk of prostate cancer.“Controlled for age, race, and body mass index, symptomatic BPH was not associated with PC risk.
The study published in “The Journal of Urology” (Newton MR et al., 2010) analyzed 2,880 patients who did surgical treatment for prostate cancer and found an inverse relationship between BPH and prostate cancer. The likelihood of high-grade PC is reduced by about 15% across the lowest vs. highest prostate sizes. Moreover, some other studies found that PC from larger glands have a more favorable Gleason score (P<.0001), lesser tumor volume, and lower chances of invasion from the gland (P<.0001) (Hong SK et al., 2014). Thus, most studies support more favorable PC outcomes for larger versus more minor prostate glands.
The Larger the Central Gland, the Lower the Risk of Prostate Cancer
The volume and thickness of CG and PZ evaluated by MRI were compared with pathological characteristics obtained from a biopsy or prostatectomy to examine the relationship between prostate size and prostate cancer risk (K. R. Nandalur et al., 2021). A total of 405 men who had prostate pathology via prostatectomy or biopsy were included in the study within six months after MRI.
Prostatectomy and prostate biopsy analyses revealed the absence of progressive pathology (Grade Group 1 (GG1) in 178 and adverse pathology (defined as ≥Grade Group 2 (GG2) in 227 patients. Moreover, the multifocal disease was present in 180 patients. No significant baseline difference between the groups was found concerning age, body mass index, PSA, or race.
The Results of The Study
As shown in the Table, the negative (GG1) group had significantly higher Total, Central Gland, and Peripheral Zone volumes than those of adverse GG ≥ 2. Central Gland volume was independently associated with lower odds of prostate cancer with OR (odds ratio) 0.97 (95% CI 0.96–0.98) (p < 0.0001), which confers an approximately 3% decrease in risks for GG ≥ 2 for a one cc increase in CG volume.
| Negative/Grade group 1 (n = 178) | Grade Group ≥ 2 (n = 227) | p-value | |
| Total prostate volume (cm3) | 63.8 (37.6) | 41.7 (21.6) | <0.001 |
| Central gland volume (cm3) | 44.2 (35.6) | 24.0 (19.5) | <0.001 |
| Peripheral zone volume (cm3) | 19.6 (8.3) | 17.7 (7.5) | 0.01 |
| Mean thickness PZ (mm) | 6.7 (2.2) | 7.2 (2.2) | 0.02 |
A similar association was found for the multifocal disease. CG volume was linked with lower chances of multifocal disease with an OR of 0.97 (95% CI 0.96–0.98) (p < 0.0001). Despite being the primary site of PC origin, the volume and thickness of the PZ were associated neither with GG ≥ 2 nor multifocal disease.
The results of this study support a robust inverse association between prostate size and the risk of significant PC. Moreover, they also discovered that Central Gland volume, not Peripheral Zone characteristics, reduces PC chances. A global mechanism from the central gland volume drives the potential protective effects of an enlarged prostate.
Should We Reduce the Size of the Prostate to Alleviate the BPH Symptoms?
Given the results, the treatment of BPH to decrease CG volume comes into question. It is a known fact that androgens are involved in developing prostate cancer. 5-alpha-reductase inhibitors (Finasteride and Dutasteride) can prevent the conversion of testosterone into its more potent form, dihydrotestosterone, which may reduce the risk of PC.
The 2003 Prostate Cancer Prevention Trial (Thompson IM et al., 2003) showed a decreased risk of PC but also a higher risk of high‐grade disease with 5‐alpha‐reductase inhibitors. The trial involved 18,882 men 55 years of age or older. Treatment with finasteride (5 mg per day) for seven years resulted in a 25% reduction in prostate cancer prevalence (P<0.001). However, tumors of advanced Gleason grade were more common in the finasteride group (37.0%) than the placebo group (22.2%), with P<0.001.
The authors also noted that sexual side effects were more common in finasteride-treated men, whereas urinary symptoms were more common in men receiving a placebo. So, despite 5-alpha-reductase inhibitors blocking to some extent the appearance of PC and reducing the risk of urinary problems, one should weigh these benefits against more severe sexual side effects and the higher risk of high-grade prostate cancer.
5-ARIs used to treat BPH may reduce serum PSA concentrations by 50%, thereby hiding the accurate picture of prostate cancer development. Furthermore, a recent study has found worse pathologic outcomes and higher PC‐specific mortality with 5‐alpha‐reductase inhibitor use (Sarkar RR et al., 2019). This study showed that 5-AR inhibitors delayed diagnosis and worse cancer-specific outcomes in men with PC. The study concluded: “These data highlight a continued need to raise awareness of 5-ARI-induced PSA suppression, establish clear guidelines for early prostate cancer detection, and motivate systems-based practices to facilitate optimal care for men who use 5-ARIs.”
Conclusions
Given their symptoms, people often confuse BPH and prostate cancer and believe increased size is due to pathologic growth. However, recent research suggests that these are entirely different entities, and even more, an enlarged prostate appears to have a lower chance of significant PC. The age-related enlargement of the prostate is a sign that your body is protecting your prostate from PC. Interrupting this natural process with chemical drugs is probably not the best solution. Moreover, studies show that such interventions often fail.
References
- K. R. Nandalur et al. MD. (2021) Benign prostate hyperplasia as a potential protective factor against prostate cancer: Insights from a magnetic resonance imaging study of compositional characteristics. The Prostate Volume 81, Issue 14 p. 1097-1104.
- Schenk JM, Kristal AR, Arnold KB, et al. Association of symptomatic benign prostatic hyperplasia and prostate cancer: results from the prostate cancer prevention trial. Am J Epidemiol. 2011;173(12):1419‐1428.
- Newton MR, Phillips S, Chang SS, et al. Smaller prostate size predicts high grade prostate cancer at final pathology. J Urol. 2010;184(3):930‐937.
- Hong SK, Poon BY, Sjoberg DD, Scardino PT, Eastham JA. Prostate size and adverse pathologic features in men undergoing radical prostatectomy. Urology. 2014;84(1):153‐157.
- Thompson IM, Goodman PJ, Tangen CM, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med. 2003;349(3):215‐224.
- Sarkar RR, Parsons JK, Bryant AK, et al. Association of treatment with 5α‐reductase inhibitors with time to diagnosis and mortality in prostate cancer. JAMA Intern Med. 2019;179(6):812‐819.









As a male I find this content to be very helpful. Definitely adding your site to my bookmarks so that I can refer to it later.
I have never had a prostrate exam. I’m in my early 30s and my doctor hasn’t suggested it yet. At what age should a male start to get prostrate checks? Are there any early sings someone in their 30s could be on the lookout for?
Its always good to stay ahead of the game if you can! Great article!
Hi Conner,
I’m glad you found the article helpful! Generally, prostate exams are recommended starting at age 50 for most men, but those with a family history of prostate cancer or other risk factors have to start earlier, around 40 or 45. In your 30s, it’s less common but staying informed is wise. Early signs to watch for include urinary issues or changes, but these can often be related to other non-cancerous conditions. Always best to discuss with your doctor for advice.
Best regards,
Makhsud