Last Updated on September 4, 2025 by Max
Introduction
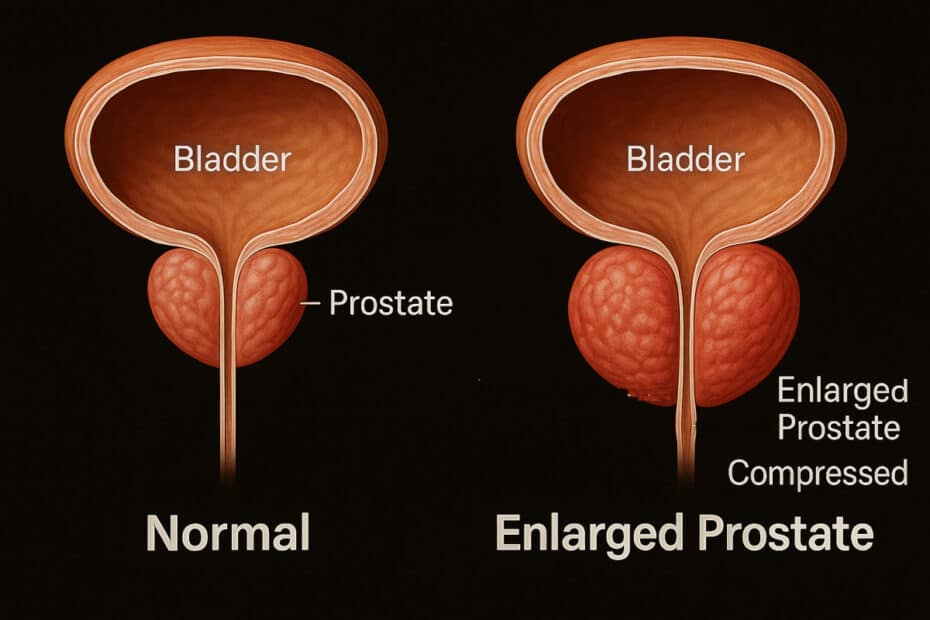
The prostate is often overlooked—until it starts to grow. Beginning the size of a walnut, this gland sits just below the bladder, surrounding the urethra. As men age, it may enlarge, sometimes doubling or tripling in volume. This condition, known as benign prostatic hyperplasia (BPH), gradually narrows the urinary channel and increases pressure on the bladder outlet. Nearly half of men over 60 report lower urinary tract symptoms, such as slow stream, urgency, and nighttime urination (Barry, M.J., 2020). To help you see why these changes occur, we’ve created an interactive slider that shows how prostate growth reshapes the urinary pathway.
Interactive Tool: BPH Progression Slider
👉 Try it yourself below: slide from “normal” to “enlarged” to watch the prostate press against the bladder and urethra, while the metrics update in real time.
(Embed full slider HTML here)
BPH Progression Slider
Slide from normal to enlarged to see how prostate growth narrows the urethra and presses on the bladder outlet. Educational model only.
References (educational ranges): Barry, M.J., 2020; Gravas, S., 2022; Irwin, D.E., 2020; Roehrborn, C.G., 2008.
Disclaimer: This tool is for educational purposes only. It simplifies complex anatomy and does not replace medical advice.
Why the Prostate Blocks the Flow
The prostate gland encircles the urethra like a clamp around a straw. When small, the urethral channel stays open and urine flows easily. But even moderate growth—rising from 20 grams to 40 grams—narrows the passage enough to cut flow rates almost in half. Doctors often measure Qmax, the maximum urinary flow rate. A healthy young man usually records ≥15 mL/s. As the gland enlarges, Qmax may fall to 7–10 mL/s, matching what you see in the slider visualization (Gravas, S., 2022). This “bottleneck effect” explains why men with BPH often describe hesitancy, dribbling, or the feeling of incomplete emptying.
From Slow Stream to Sleepless Nights
The bladder sits just above the prostate. As the gland enlarges, it pushes upward, reshaping the bladder neck. This increases outlet resistance, forcing the bladder muscle to work harder. Over time, that strain leads to irritative symptoms. One of the most frustrating consequences is nocturia—waking up at night to urinate. By their 70s, nearly 70% of men report this issue (Irwin, D.E., 2020). The slider models this by showing a rising risk as prostate size moves from mild to severe. The IPSS symptom score, used worldwide in urology clinics, categorizes symptom burden as mild, moderate, or severe. Your slider tracks this progression, giving a sense of how anatomy links to daily life.
How BPH Progresses Over Time
BPH is not the same for everyone. On average, the prostate enlarges by about 1.6 mL per year, but some men remain stable for decades while others progress rapidly (Roehrborn, C.G., 2008). Large prostates (>40 grams) are more likely to cause bothersome symptoms, urinary tract infections, or even acute urinary retention. Still, growth patterns vary, which is why visual tools like this help illustrate what’s happening inside.
What To Do If You Notice Symptoms
While the slider gives you a glimpse of the mechanism, it’s important to monitor your own health. If you notice urinary symptoms:
- Track your experiences: You can complete the IPSS questionnaire online to quantify symptom severity.
- Discuss with your doctor: A PSA blood test and digital rectal exam are standard evaluation tools.
- Adopt helpful lifestyle strategies: Reducing caffeine or alcohol, timing fluid intake earlier in the day, and regular exercise often ease the burden.
If symptoms progress or quality of life declines, medical treatments range from medications that relax or shrink the prostate to minimally invasive procedures.
👉 Curious how lifestyle changes play a role? Try our Lifestyle Impact Simulator to see the modeled effects of daily habits.
References
- Barry, M.J., 2020. Epidemiology and natural history of benign prostatic hyperplasia. Urology Journal.
- Gravas, S., 2022. Guidelines on the management of non-neurogenic male lower urinary tract symptoms. European Association of Urology.
- Irwin, D.E., 2020. Prevalence of nocturia and its impact. BJU International.
- Roehrborn, C.G., 2008. Pathophysiology of benign prostatic hyperplasia progression. Reviews in Urology.