Last Updated on July 7, 2024 by Max
Introduction
Benign prostatic hyperplasia (BPH) or prostate enlargement develops in men over the age of 40 and may cause lower urinary tract symptoms (LUTS). In Europe, 30% (26 million men) and in the USA, 8 million men over 50 years of age are affected by LUTS. Besides LUTS, BPH can cause serious health issues too: acute urinary retention, bladder stones, urinary tract infection, hematuria, renal insufficiency, and upper urinary tract atrophy.
Any website of the medical clinic trying to emphasize the benefits of the techniques available at this facility often downplays the negative aspects of the procedure. Therefore, distributing the advantages and side effects of different ways of BPH treatments using clinical study results may play an important role in decision-making between patients and their healthcare providers.
The First Evaluation of BPH
The first evaluation of BPH includes:
- medical history: to find the potential causes and relevant comorbidities,
- symptom score questionnaires (e.g., the IPSS (International Prostate Symptom Score)): to assess urinary symptom severity and quality of life,
- digital rectal examination: to determine the size of the prostate and the possible coexistence of prostate cancer,
- urinalysis: for differential diagnosis of urinary tract infection,
- prostate‐specific antigen (PSA) test: for detection of prostate cancer, would be performed if life expectancy is greater than ten years,
- and frequency volume chart: the recording of volume and time of each void by the patient.
Initial Treatments For BPH
Initial treatments for BPH include:
- conservative: watchful waiting and lifestyle change: 87% of men who have chosen watchful waiting experience a worsening of symptoms over four years;
- medication, such as alpha‐blockers (tamsulosin-brand name Flomax ) and 5‐alpha reductase inhibitors (finasteride-brand names Proscar and Propecia and Dutasteride-brand name Avodart). About half of patients on medications do not have significant improvement in symptoms (< 4 point IPSS improvement).
Prostate surgery is the choice if a man cannot get relief through conservative medical treatment or BPH causes the complications mentioned above.
Until the 1970s, open prostatectomy and endoscopic removal of prostatic tissue or transurethral resection of the prostate (TURP) were the only choices to relieve LUTS.
Open Prostatectomy
At an open prostatectomy, a cut is made in the tummy area through which the outer part of the prostate is removed. Open surgery is rarely recommended nowadays and only in the case of an extremely large prostate. It has the highest risks of long-term complications, such as urinary incontinence and erectile dysfunction.
Transurethral Resection of the Prostate
TURP is carried out with a resectoscope, which is a tube with a camera, light, and a wire loop to cut the prostate tissue. At TURP, no cuts to the skin are made; the resectoscope gets to the prostate along the urethra. The prostate tissue cutting is performed by electrocautery or sharp dissection. TURP takes about 90 minutes and is done under local or general anesthetic. Men who have had TURP usually stay in the hospital for two to seven days and use a special tube to remove pee from the bladder. How long he will stay off work depends on the kind of his job; he needs to stay away from strenuous work for a few weeks. The procedure might have to be repeated after a while.
The European Association of Urologists recommends TURP for prostates between 35 and 80 ml, and open prostatectomy remains the only option for prostates exceeding that limit. Despite these recommendations, there is enough data to support TURP for prostates over 100 ml.
In a study by Persu et al. (2010), 200 patients with large prostates (up to 160 ml) were randomized equally into two arms: TURP and Open surgery. The clinical study showed that TURP might lead to similar results in skillful hands while keeping the complication rate low and obtaining shorter hospitalization times and lower costs.
Advantages of the TURP
TURP is a well-elaborated technique with predictable outcomes and is considered a golden standard to relieve the symptoms of LUTS related to BPH. Therefore, knowing which outcomes this golden standard provides to the patients is good. In an analysis of 20 randomized controlled studies published between 2005 and 2009 and a maximum follow–up of 5 years, TURP resulted in:
- improvement of the maximum urinary flow rate, Qmax (162%),
- reduction of the International Prostate Symptom Score, IPSS (–70%),
- reduction of the quality of life (QoL) score (–69%),
- reduction of the post-void residual urine volume (–77%).
Generally, the outcome of TURP performed for LUTS is favorable in 78–93% of patients.
Usually, it takes a few months to get total control, during which you may still have some urinary problems; the body needs time to adapt to the operating area changes and start working normally again.
For example, about 75 % of men only have mild symptoms nine months after having TURP. In another study, an interview of 280 men 12 years after they had a TURP showed that only 13 % were unsatisfied with the results of the surgery.
Disadvantages of the TURP
The most common complication of a TURP is retrograde ejaculation or dry orgasm when the sperm flows into a bladder rather than getting outside through the urethra. Retrograde ejaculation is caused by damage to nerves and muscles in the neck of the bladder junction area between the bladder and prostate. At the moment of ejaculation, the bladder neck muscles tightly close the urethra, thus preventing sperm from getting into the bladder. An estimated 70% to 90% of men have this side effect after TURP. It doesn’t affect sexual pleasure during orgasm but reduces fertility.
Urinary incontinence is quite common after TURP, but usually, it gets better during the rehabilitation time after the surgery. However, sometimes it can be a long-term problem and require medication or surgery.
Erectile dysfunction can be either temporary or permanent and affects from 10% to 20% of men after TURP. Usually, it is a short-term problem that resolves during a recovery period.
Narrowing of the urethra (urethral strictures) is one more negative side effect of TURP that may sometimes need surgery. It is estimated to develop in up to 4% of TURP cases due to the scarred urethra.
TUR syndrome is a rare complication of TURP (about 1-3%) but may be related to life-threatening risk. It develops if too much of the fluid used in the surgery area gets into the bloodstream. Nausea, vomiting, or confusion are common symptoms of TUR syndrome, but in rare cases, it can cause cardiovascular problems.
Some of the other risks of TURP include:
- bleeding – in around 2% of cases;
- urinary tract infection is treated with antibiotics in around 5% of cases.
- About 10% of men need to have a TURP again within ten years.
These TURP surgery issues have stimulated the development of minimally invasive procedures:
- laser ablation or enucleation,
- microwave thermotherapy,
- radiofrequency,
- high‐intensity focused ultrasound,
- water vapor therapy,
- mechanical devices (prostatic stent, prostatic urethral lift),
- fractionation of prostatic tissue (Aquablation),
- prostate artery embolization,
- intraprostatic drugs.
Definitions
International Prostate Symptom Score (IPSS) is based on the answers to seven questions concerning urinary symptoms and one question concerning quality of life. You can choose one point from 0 to 5, so the total score can therefore range from 0 to 35 (asymptomatic to very symptomatic). . Mild symptoms: 0 to 7; moderate symptoms: 8 to 19; severe symptoms: 20 to 35.Quality of life (QoL) score in the context of BPH diagnosis presumes to answer the only question: “If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about that? Answers: 0 – Delighted, 1 – Pleased, 2 – Mostly Satisfied, 3 – Mixed, 4 – Mostly Dissatisfied, 5 – Unhappy, 6 – Terrible.The urinary flow rate (Qmax) is the volume of urine excreted per second or per minute. Qmax indicates the maximum flow rate. A lower Qmax may indicate that the enlarged prostate puts pressure on the urethra. The International Index of Erectile Function (IIEF) Questionnaire is a 15-question validated investigation that has been found useful in the clinical assessment of erectile dysfunction. A score of 0-5 is awarded to each of the 15 questions that examine the four main domains of male sexual function: erectile function, orgasmic function, sexual desire, and intercourse satisfaction.
Laser Ablation or Enucleation
Laser ablation or enucleation uses a holmium laser (HoLAP or HoLEP) to cut away excess prostate tissue. HoLEP, like TURP, is performed through the urethra and has been estimated to be as invasive well as effective as TURP.
Advantages of the HoLEP
At laser ablation, the cut area bleeds less, so the patients can leave the hospital and have their catheter used for bladder draining removed sooner than at TURP. Another advantage of the HoLEP technique is that there is no risk of TUR syndrome.
Transurethral Vaporization of the Prostate (TUVP)
Transurethral vaporization of the prostate (TUVP) includes bipolar electrosurgical vaporization or laser vaporization techniques. At laser vaporization, a tube called a cystoscope is inserted into the urethra, and laser energy is used to burn away prostate tissue.
Advantages of the TUVP
- The results of TUVP in terms of the degree of symptom relief are entirely comparable to that of TURP.
- Vaporization is safer than traditional TURP.
- The procedure runs almost without bleeding, so a doctor can see clearly what he is doing.
- Short catheterization time; most patients (95%) go home the same day.
- Shorter procedure time (65-70 min).
- Lower rates of erectile dysfunction than with TURP because there’s no electric current outside of the prostate, potentially injuring the cavernosal nerves.
Disadvantages of the TUVP
- Blood in the urine, but less than at TURP.
- Irritation of the urethra, burning sensation during urination.
- Frequent urination.
- Bladder irritation.
- Retrograde ejaculation (about 30-50%).
In a comparative study of HoLAP and TUVP, the authors concluded that holmium laser ablation and photoselective vaporization of the prostate are safe and effective in patients with BPH with a small to moderate size prostate (up to 60 cc). Both procedures are easy to learn, but holmium laser ablation of the prostate requires a longer operating time (69.8 vs. 55.5 minutes).
Transurethral Microwave Thermotherapy (TUMT)
Transurethral microwave thermotherapy (TUMT) is a minimally invasive procedure that can be performed under a local anesthetic on an outpatient basis.
During a TUMP procedure, the microwave antenna inserted through the urethra emits microwaves to heat and destroy the surrounding prostatic tissue. It can take 30-60 minutes and is well tolerated by patients.
The main disadvantages of TUMP include:
- Urinary retention
- Infection
- Retrograde ejaculation
- Intense pain during the procedure
- Urination pain for several weeks
The European Association of Urology (EAU) has removed TUMP from its guidelines. The American Urological Association (AUA) guidelines state that patients should be informed about the associated with the TUMP higher risk of necessary retreatment compared to TURP.
Water Vapor Thermal Therapy (WVTT or Rezum)
Water vapor thermal therapy (WVTT or Rezum) is a minimally invasive surgical procedure that uses steam, which is delivered transurethrally into the transition zone of the prostate. Depending on the size of the prostate, an adequate number of injections is made into the middle and upper sites of the prostate without injuring the prostatic part of the urinary tube. The cells, contacted with the vapor die immediately. The body gradually removes the dead cells for about three months, thus shrinking the prostate and relieving BPH. WVTT was approved by the United States Food and Drug Administration in 2015.
The most recent analysis of the WVTT efficacy by Miller et al. (2020) included five cohort studies comprising 514 patients. The mean prostate volume across the studies ranged from 45 to 53 ml. Follow-up time varied in each study and ranged from 6 to 48 months. All WVTT surgeries were successfully completed without procedure-related complications.
Advantages of the WVTT
- Symptom improvement after the WVTT exceeded published minimal clinically important difference by several-fold over four years of follow-up,
- Low rate of surgery retreatment; 7% at four years follow-up.
- The procedure didn’t affect the erectile function of the patient; there were no reports of de novo ED (Fig.).
- There are no side effects associated with bleeding; removal of the dead cells happens naturally and takes about three months.
- Short procedure time; less than 60 minutes;
Disadvantages of the WVTT
The main adverse events at WVTT were:
- Dysuria (16.2%)
- Urinary retention (11.2%)
- Urinary tract infection (10.9%)
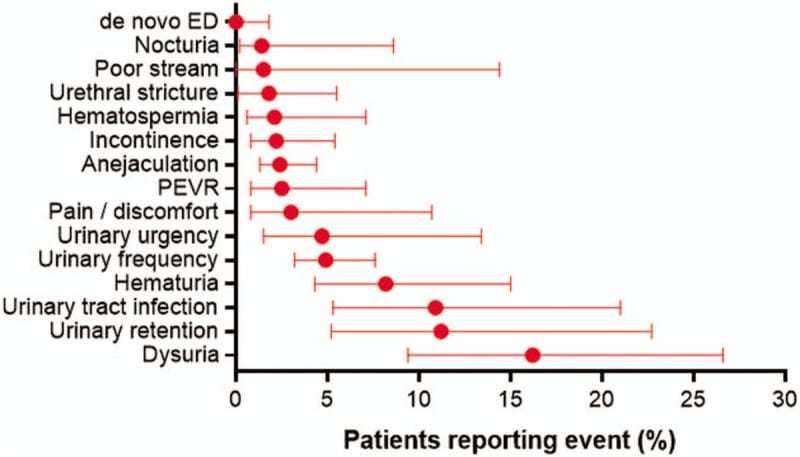
Most registered complications were nonserious and transient.
Water vapor thermal therapy was tested and appears to work on larger prostates exceeding 80 mL in size (Pham H, Sharma P (2018)).
Men with severe LUTS are usually unwilling to do surgery due to adverse events related to anesthetic risk and sexual side effects. WVTT has been used lately with a growing rate to treat men with bothersome BPH symptoms who wish to avoid invasive surgery while preserving sexual function.
Prostatic Urethral Lift (PUL)
Prostatic urethral lift (PUL) is a minimally invasive therapy that treats BPH by lifting and holding the prostate tissue out of the way, thus clearing the urethral tube for urine passage. To achieve this, typically, four implants are placed into the prostate, and no heating, cutting, or removal of the prostate tissue is required.
In 2015, The National Institute for Health and Care Excellence (UK) conducted an independent review of clinical data on UroLift and made the following recommendation: “The Committee concluded that the UroLift system is effective in relieving symptoms of benign prostatic hyperplasia. It noted that the degree of symptom relief outcomes is slightly less than that of TURP or holmium laser enucleation (HOLEP), but it is sufficient and clinically important.”
To assess the effectiveness of the UroLift System, a randomized, sham-controlled, and blinded study comprising 19 centers (14 in the USA, 3 in Australia, and 2 in Canada) was conducted (2016). The upper limit for prostate size was 80 ml.
Post-operative events reported in the LIFT study: PUL vs. sham
| Event | UroLift group (%) | Sham group (%) |
|---|---|---|
| Dysuria | 34 | 17 |
| Haematuria | 26 | 5 |
| Pelvic pain | 19 | 9 |
| Urge incontinence | 7 | 8 |
| Urinary tract infection | 3 | 2 |
The following conclusions are the main results of the study analysis:
- Most adverse events detected in the PUL studies were moderate that typically resolved within two weeks; no large irritative symptoms characteristic of thermal ablation were observed.
- No reports of bleeding requiring transfusion.
- No urinary incontinence following PUL.
- Catheterization time was less than one day; 68% of the patients were able to avoid catheterization.
- The duration of the hospital stay was under a day.
- No adverse impact on sexual function; on the contrary, those patients who had reported severe erectile dysfunction before the study reported modest improvement after the procedure.
- no reports of retrograde ejaculation.
- PUL procedure maintained the improvements of LUTS relief, quality of life, and uroflow for over four years.
- retreatment rates were 5% at one year, 10.7% at three years, and 13.6% at four years.
- All US-based study participants were treated using a local anesthetic, transurethral lidocaine.
WVTT and PUL are the only alternatives to TURP recommended by the American Urological Association for those who want to have their sexual function unaffected.
So, eventually have two minimally invasive therapies, WVTT and PUL procedures pretending to be “ideal” in terms of LUTS relief, quality of life, and uroflow improvement.
While no direct comparison studies have been conducted, some reviews of WVTT and PUL effectiveness in the literature can be used for their indirect comparison.
| UroLift | WVTT |
|---|---|
| In a review by Perera M. et al. (2015) of PUL results at 1 year | In a review by Miller et al. (2020) of WVTT results at 1 year |
| IPSS decreased by 8.0 points | IPSS decreased by 11.1 points |
| QOL (Quality of Life) decreased by 2.2 points | QOL decreased by 2.2 points |
| Qmax (uroflow) improved by 3.8 mL/s | Qmax improved by 5.1 mL/s. |
| Over five years of follow-up of PUL patients (Roehrborn CG. et al. (2017) | Over four years of follow-up of WVTT patients (McVary, 2019) |
| 32 of 140 (22.9%) had to repeat a surgery (19 for LUTS and 13 for implant removal) | Only 6 of 135 (4.4%) underwent surgical retreatment (all for LUTS) |
| The percentage of patients who restarted BPH medications was 9.3% with PUL. | The percentage of patients who restarted BPH medications was 5.2% with WVTT. |
Taken together treatment effectiveness, retreatment rate, and cost of the procedure, PUL proved to be more expensive and less effective than WVTT (Ulchaker JC, Martinson MS. 2019).
Prostatic Artery Embolization (PAE)
PAE is a non-surgical, minimally invasive therapy involving stopping the blood supply of the prostate tissue by injection of tiny beads into the prostatic arteries. The reduced blood supply, in turn, causes the shrinking of the prostate gland and relieves LUTS. Although the first trial results were published 20 years ago and increasing research on PAE, the use of the technique remains at an incipient stage.
Kuang et al. (2017) reviewed ten studies representing 788 patients. At 24 months of follow-up, prostate volume, PSA, Qmax, IPSS, and QoL were significantly improved (P < 0.05). The international index of erectile function ((IIEF-5)) was unchanged at 6 and 12 months but was significantly reduced at 24 months.
Malling et al. (2019) reviewed 13 studies representing 1,254 patients with a mean IPPS of 23.5. PAE improved IPSS by 67%. At the 12-month follow-up, all other study outcomes, including QoL, IIEF-5, prostate volume, PSA, Qmax, and post-void residual, were improved as well. Major complications were reported in 0.3% of the cases.
In 2018 Ray et.al. summarised the results of a large comparative study of PAE and TURP comprising 305 patients, 216 of whom underwent PAE and 89 of whom underwent TURP. The trials showed that PAE produced a reduction of IPSS by 10-point at 12 months post-procedure. However, PAE did not appear to be as effective as TURP, which resulted in a reduction of IPSS by 15-point at the same follow-up period. In terms of IPSS and quality-of-life improvement, there was no evidence of PAE being non-inferior to TURP. Patients in the PAE group had a reoperation rate of 5% before 12 months and 15% after 12 months (20% total rate).
| Advantages of PAE | Disadvantages of PAE |
|---|---|
| Low complication rate: of 216 patients, one had sepsis, four had local arterial dissection, four had a groin hematoma, and two patients had non-target embolization, which resulted in penile ulcers. | The procedure involves extensive imaging, which may result in significant radiation exposure. |
| 71% of PAE cases were performed as outpatient or day cases; In contrast, 80% of TURP cases required at least one night of hospital stay, and the majority required two nights. | Although PAE provides significant improvements in key target indicators, including the main LUTS symptoms, quality of life, and uroflow dynamics, comparative improvement in these signs is inferior to other minimally invasive therapies. |
| Avoiding a general anesthetic. | The most common adverse effects of PAE include acute urinary retention, rectal bleeding, pain, blood in the urine/sperm, and urinary tract infection. Serious complications are uncommon and include arterial dissection, bladder wall ischemia, and persistent urinary tract infection. |
The place of PAE in the treatment of LUTS caused by BPH is considered between that of drugs and surgery, thus allowing the doctor more flexibility in meeting the requirements of the patients and considering individual symptoms and anatomical variations.
Which Approach to Choose?
If you have to decide which approach is the best option for you, discuss with your doctor the advantages and risks of the different types of surgeries. The decision will depend on the size of your prostate, your age, and your health status. Bear in mind some external factors, such as the availability of the specific technique at your local hospital and the surgeon’s level of experience that may affect the final decision.
References
- European Association of Urology. Treatment of non‐neurogenic male LUTS. uroweb.org/guideline/treatment‐of‐non‐neurogenic‐male‐luts/ (accessed 1 March 2018).
- Benign enlarged prostate: What are the pros and cons of surgery? 2008 Oct 13 [Updated 2018 Jan 25]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK481492/
- Daimantas M, et al. (2015). The effect of complete transurethral resection of the prostate on symptoms, quality of life, and voiding function improvement. Cent European J Urol. 2015; 68(2): 169–174.
- C Persu et al. TURP for BPH. How Large is Too Large? J Med Life. 2010 Nov 15; 3(4): 376–380.
- E. A. Elzayat et al (2009) Holmium laser ablation of the prostate versus photoselective vaporization of prostate 60 cc or less: short-term results of a prospective randomized trial. J Urol. 2009 Jul;182(1):133-8.
- L. E. Miller et al. (2020) Water vapor thermal therapy for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Medicine (Baltimore). 2020 Jul 24; 99(30): e21365.
- Pham H, Sharma P (2018). “Emerging, newly-approved treatments for lower urinary tract symptoms secondary to benign prostatic hypertrophy”. Can J Urol. 25 (2): 9228–9237.
- NICE Guidance: UrolLift for treating lower urinary tract symptoms of benign prostatic hyperplasia. Published date: September 2015.
- Roehrborn CG. Prostatic Urethral Lift: A Unique Minimally Invasive Surgical Treatment of Male Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia. Urol Clin North Am 2016;43:357-69.
- Perera M, Roberts MJ, Doi SA, et al. Prostatic urethral lift improves urinary symptoms and flow while preserving sexual function for men with benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Urol 2015;67:704–13.
- Roehrborn CG. et al (2017). Five year results of the prospective randomized controlled prostatic urethral L.I.F.T. study. Can J Urol. 2017 Jun; 24(3):8802-8813.
- McVary KT, Rogers T, Roehrborn CG. Rezum water vapor thermal therapy for lower urinary tract symptoms associated with benign prostatic hyperplasia: 4-year results from randomized controlled study. Urology 2019;126:171–9.
- Ulchaker JC, Martinson MS. Cost-effectiveness analysis of six therapies for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. Clinicoecon Outcomes Res 2018;10:29–43.
- Kuang, M., Vu, A. & Athreya, S. A Systematic Review of Prostatic Artery Embolization in the Treatment of Symptomatic Benign Prostatic Hyperplasia. Cardiovasc Intervent Radiol 40, 655–663 (2017).
- B Malling et al. (2019) Prostate artery embolisation for benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Radiol. 2019 Jan;29(1):287-298.
- Alistair F Ray et.al. (2018) Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: an observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int. 2018 Aug;122(2):270-282.