Last Updated on September 4, 2025 by Max
Introduction
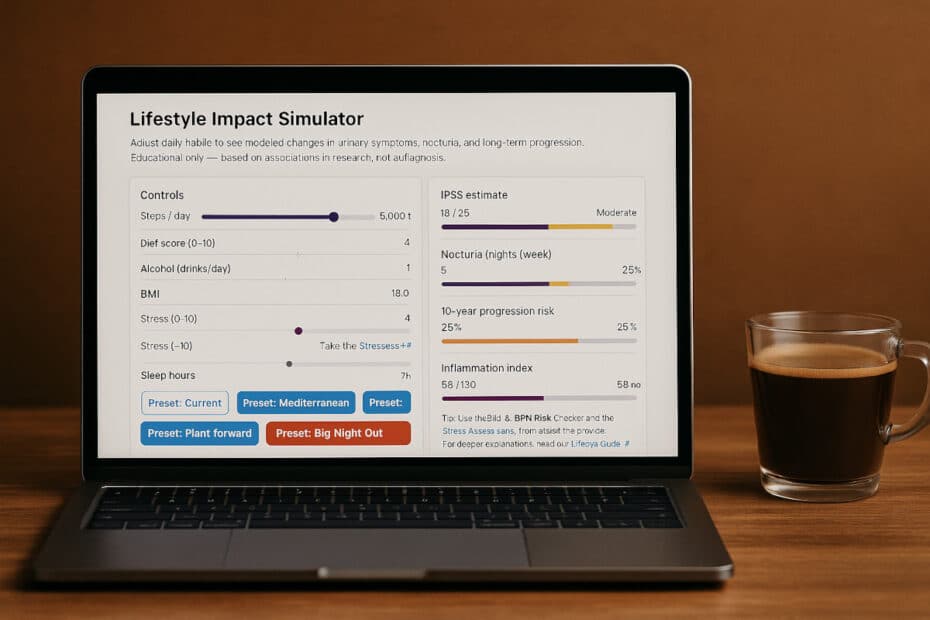
Everyday decisions—how often you move, what you eat, whether you enjoy that late-night drink—leave fingerprints on prostate health. While no single habit guarantees protection, large clinical studies show that consistent lifestyle patterns influence urinary symptoms, the pace of prostate enlargement, and the risk of long-term complications. Men often underestimate how much agency they have. Our Lifestyle Impact Simulator offers a visual way to explore these connections. With each toggle, you can see modeled changes in symptom scores, urinary flow, and nocturia risk, based on published research.
Interactive Tool: Lifestyle Impact Simulator
Lifestyle Impact Simulator
Adjust daily habits to see modeled changes in urinary symptoms, nocturia, and long-term progression. Educational only — based on associations in research, not a diagnosis.
Tip: Use the BMI & BPH Risk Checker and the Stress Assessment, then revisit the presets.
For deeper explanations, read our Lifestyle Guide . This simplified educational model reflects associations reported in research and summarized in your lifestyle guide. It is not medical advice.
Disclaimer: This simulator illustrates associations found in research on prostate health. It simplifies complex biology and is for educational purposes only. It is not a diagnostic or medical tool.
Why Lifestyle Matters
Epidemiological studies leave little doubt about the connection between lifestyle and lower urinary tract symptoms. In one long-term study, men who walked briskly for at least two hours per week had about a 25 percent lower risk of BPH progression compared with those who remained sedentary (Parsons, J.K., 2008). Another investigation showed that men with a BMI over 30 were nearly twice as likely to develop severe symptoms compared with men at a healthy weight (Egan, K.B., 2016). These are not abstract numbers. They explain why some men in their sixties still sleep through the night, while others are up two or three times before dawn.
The Role of Diet and Inflammation
Nutrition plays an equally important role. Diets heavy in red meat, dairy, and processed foods correlate with a greater risk of nocturia and urgency. On the other hand, men who eat more vegetables, fruits, and omega-3-rich foods experience slower symptom progression and fewer nighttime episodes (Maserejian, N.N., 2011). The underlying mechanism is thought to involve systemic inflammation. Metabolic factors such as obesity, insulin resistance, and low-grade inflammation amplify growth signals inside the prostate. This biological link explains why diet quality affects a gland that most men never even think about until problems arise.
Alcohol, Caffeine, and Sleep
Alcohol and caffeine exert their effect through bladder irritation. A glass of wine in the evening may not matter in youth, but as the bladder becomes more sensitive with age, those late drinks often translate into nocturnal urgency. Clinical surveys show that men who reduce caffeine and alcohol report measurable improvements in sleep continuity and quality of life. Since up to 70 percent of men over seventy experience nocturia, even small adjustments in habits may determine whether nights are restful or interrupted (Irwin, D.E., 2020).
What the Simulator Shows
When you select more daily steps, a better diet, or reduced alcohol intake in the simulator, the model recalculates your International Prostate Symptom Score (IPSS), your risk of nocturia, and your expected ten-year progression curve. The outputs are based on pooled data: IPSS typically improves by 3–4 points in men who combine exercise and dietary changes, enough to shift from moderate into mild territory. Nocturia risk declines by 20 to 30 percent in men who maintain a healthy weight and avoid bladder irritants. And although prostate growth itself is not halted, progression slows, reducing the likelihood of invasive procedures.
Taking Action
The simulator emphasizes that lifestyle is not a cure, but rather a trajectory shifter. Just as hypertension is influenced by diet and exercise, so too are urinary symptoms shaped by daily behavior. Even if symptoms have already started, changing habits today alters what the next decade looks like. This message is important: it is never too late to benefit.
References
- Parsons, J.K., 2008. Physical activity, obesity, and the risk of benign prostatic hyperplasia. European Urology.
- Egan, K.B., 2016. The epidemiology of benign prostatic hyperplasia. Nature Reviews Urology.
- Maserejian, N.N., 2011. Dietary patterns and lower urinary tract symptoms in men. American Journal of Epidemiology.
- Irwin, D.E., 2020. Prevalence of nocturia and its impact. BJU International.