Last Updated on July 7, 2024 by Max
Introduction
Chronic pelvic pain syndrome has long been misunderstood and often overlooked, leaving countless individuals silently enduring the physical and emotional burdens it brings. In a world where healthcare advances continue to push boundaries, we shine a light on this invisible enemy and explore the intricacies surrounding its diagnosis, treatment, and management.
As you embark on this educational journey, you’ll discover how chronic pelvic pain syndrome affects people from all walks of life, their challenges in obtaining a proper diagnosis, and the many available treatments that can lead to improved quality of life. This blog post strives to provide a comprehensive overview of the condition while offering hope and support to those who grapple with its effects. Get ready to dive deep into the world of chronic pelvic pain, and together, let’s take steps to demystify and ultimately defeat this invisible enemy.
- Introduction
- Understanding Chronic Pelvic Pain Syndrome
- Diverse and Complex Underlying Causes
- Prevalence of CPPS in Men and Women
- Navigating the Diagnostic Odyssey
- Treatment and Management Strategies
- Specialized clinics focusing on CPPS treatment
- Lessons Learned and Advice From Survivors
- The Success Rate for Chronic Pelvic Pain Syndrome (CPPS)
Understanding Chronic Pelvic Pain Syndrome
Chronic pelvic pain syndrome (CPPS) is a complex and misunderstood condition affecting both men and women. Chronic pelvic pain is defined as pain in the pelvic region lasting more than six months, affecting both men and women. In men, the condition is often referred to as chronic prostatitis or chronic pelvic pain syndrome (CP/CPPS), while in women, it may be associated with various gynecological disorders.
Symptoms of CPPS include persistent pain in the pelvic region, lower back, or genitals, which may be dull, aching, sharp, or throbbing. Other accompanying symptoms can include pain during urination, bowel movements, or sexual activity, as well as increased urinary urgency and frequency.
Diverse and Complex Underlying Causes
A. CPPS has a multifaceted etiology, which may include physical, psychological, and environmental factors. Some possible physical causes of CPPS include:
- Musculoskeletal causes: One potential cause of CPPS is dysfunction in the pelvic floor muscles. These muscles support the pelvic organs and are involved in bowel, bladder, and sexual function. Studies have shown that pelvic floor muscle tension or spasms can occur in up to 50% of men with CP/CPPS (Cornel et al., 2005).
- Inflammatory or infectious causes: Inflammation can be an underlying cause of CPPS. Sexually transmitted or urinary tract infections may also contribute to chronic pelvic pain (Clemens et al., 2007). Chronic bacterial prostatitis is estimated to account for approximately 5-10% of all prostatitis cases (Krieger et al., 2008). Nonbacterial prostatitis or prostatodynia is more common, accounting for 90-95% of cases. In women, pelvic inflammatory disease (PID) affects around 5-10% of women of reproductive age in the United States and can contribute to CPPS. (Centers for Disease Control and Prevention, 2015).
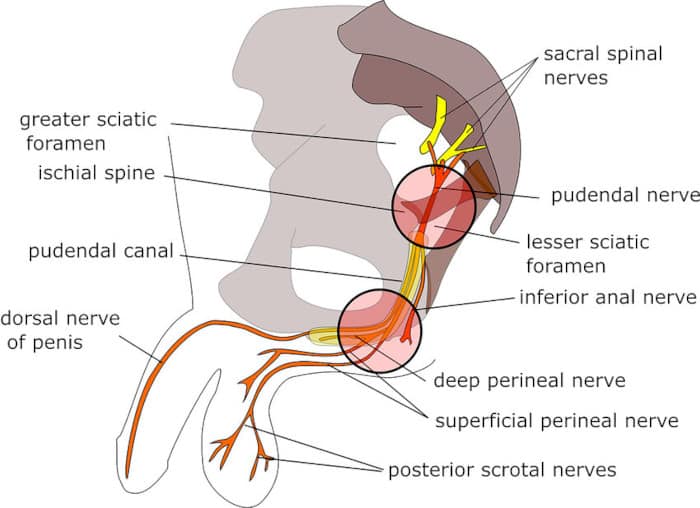
- Nerve involvement: Pudendal neuralgia, a condition in which the pudendal nerve becomes irritated or compressed, can contribute to CPPS. The pudendal nerve supplies sensation and motor function to the pelvic region, and its dysfunction can lead to chronic pelvic pain (Labat et al., 2008). The prevalence of pudendal neuralgia is considered a less common cause of CPPS than other factors.
- Hormonal imbalances.
B. Psychological factors such as stress, anxiety, or a history of trauma or abuse can contribute to developing or exacerbating CPPS. Sometimes, the pain may manifest as unresolved emotional issues or a maladaptive stress response.
C. Environmental factors, including sedentary lifestyles, poor posture, and prolonged sitting, can also contribute to the development of CPPS by increasing pressure on the pelvic region and causing muscle imbalances.
Prevalence of CPPS in Men and Women
CPPS affects both men and women, but its prevalence varies between the genders. In men, studies estimate that the prevalence of CP/CPPS ranges from 2% to 16% (Krieger et al., 2008). In women, the prevalence of chronic pelvic pain is estimated to be around 15% (Mathias et al., 1996).
The gender-specific presentation of CPPS may contribute to the differences in prevalence. In men, the condition is often associated with prostatitis, while in women, it can be related to gynecological disorders like endometriosis, pelvic inflammatory disease, or interstitial cystitis.
Understanding the complexities of chronic pelvic pain syndrome is essential for proper diagnosis and management.
Navigating the Diagnostic Odyssey
Chronic pelvic pain syndrome can be a challenging condition to diagnose and manage. In this chapter, we will explore the obstacles faced in obtaining an accurate diagnosis, the importance of multidisciplinary healthcare teams, and the critical diagnostic tests and imaging techniques used to identify the underlying causes of CPPS.
The Importance of Multidisciplinary Healthcare Teams
Given the complexity of CPPS, a multidisciplinary healthcare team can be instrumental in providing comprehensive care. This team may include the following specialists:
- urologists
- gynecologists
- physical therapists
- pain management specialists
- mental health professionals.
By working together, these healthcare professionals can address the various aspects of CPPS, ensuring that the physical, emotional, and lifestyle factors contributing to the condition are thoroughly evaluated and treated.
Critical Diagnostic Tests and Imaging Techniques
Medical history and physical examination: A detailed medical history and thorough physical examination are crucial in the initial assessment of CPPS. This may include a pelvic exam to evaluate the pelvic floor muscles and identify any areas of tenderness or discomfort.
Laboratory tests: Urinalysis, blood tests, and semen analysis (in men) are performed to rule out infections or other potential causes of CPPS. In women, tests for sexually transmitted infections or other gynecological issues may be necessary.
Imaging techniques: Depending on the suspected underlying cause, imaging techniques like ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT) scans can help visualize pelvic organs and structures. These imaging techniques can help identify abnormalities such as masses, structural issues, or inflammatory processes that may contribute to CPPS.
Treatment and Management Strategies
Chronic pelvic pain syndrome requires a comprehensive approach to treatment and management. In this chapter, we will discuss up-to-date treatment strategies, including lifestyle changes and self-care tips, the role of medications in pain management, alternative therapies and complementary medicine options, and surgical interventions and their potential benefits.
Lifestyle Changes and Self-Care Tips
- Physical activity: Regular exercise, including gentle stretching and low-impact activities like walking or swimming, can help improve blood flow and reduce muscle tension in the pelvic region (Anderson, R et al., 2011).
- Stress management: Practicing relaxation techniques, such as deep breathing exercises, mindfulness meditation, or progressive muscle relaxation, can help alleviate stress and tension that may contribute to CPPS (Anderson, R et al., 2011).
- Diet: A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and lean proteins, may help reduce inflammation and improve overall health (Rondanelli M. et al., 2015).
Medications and Their Role in Pain Management
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen, can help alleviate pain and reduce inflammation associated with CPPS (Samplaski, M. K., & Li, J., 2020).
- Antidepressants: Tricyclic antidepressants, like amitriptyline, can effectively manage chronic pain conditions, including CPPS (Anderson, R., & Goldstein, I., 2012).
- Anticonvulsants: Some anticonvulsant medications, such as gabapentin, can effectively manage neuropathic pain associated with CPPS (Baranowski, A. P. et al., 2012).
Alternative Therapies and Complementary Medicine Options
- Acupuncture: In some cases, acupuncture can relieve pain and improve a patient’s quality of life (Lee, S. H., Lee, B. C., 2009).
- Biofeedback: Biofeedback therapy can help patients learn to relax and control pelvic floor muscles, reducing pain and tension associated with CPPS (FitzGerald, M. P., et al., 2009).
- Transcutaneous electrical nerve stimulation (TENS): TENS can relieve pain in some patients with CPPS (Chen, Y. et al., 2016).
- Taking warm or hot baths can help relax the pelvic muscles and relieve chronic pelvic pain syndrome (CPPS). Adding herbs or essential oils to your bathwater can also provide therapeutic benefits. Some popular herbs and essential oils known for their relaxation and anti-inflammatory properties include Lavender, Epsom salt, Chamomile, and Eucalyptus.
- Deep penetrating light therapy, also known as low-level light therapy (LLLT) or photobiomodulation, has been studied for its potential to alleviate pain in various conditions, including chronic pelvic pain syndrome (CPPS). This non-invasive treatment uses low-level light wavelengths to stimulate cellular processes, potentially reducing inflammation and promoting tissue repair and healing.
A study by Youssef et al. (2011) investigated the efficacy of LLLT in treating patients with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). The study involved 28 patients who received a combination of LLLT and therapeutic exercises. After six weeks of treatment, the patients significantly improved pain and quality of life.
Another study by Albornoz-Cabello et al. (2017) investigated the effectiveness of low-level laser therapy in women with myofascial pelvic pain syndrome. The results suggested that laser and other physical therapy techniques significantly improved pain and functionality.
It’s essential to consult with your healthcare professional before considering any new treatment options.
Surgical Interventions and Their Potential Benefits
- Nerve blocks: In some cases, nerve blocks, such as pudendal or ganglion impair blocks, may relieve temporary pain for patients with CPPS (Labat, J. J.et al., 2008).
- Trigger point injections: Injections of local anesthetics and corticosteroids into myofascial trigger points can help alleviate pain associated with pelvic floor muscle tension in CPPS (Jarrell, J., 2014).
- Surgical intervention: In rare cases, when conservative treatments fail, and a specific underlying cause is identified, surgical intervention, such as laparoscopic resection of endometriosis or pelvic adhesions, may be necessary for women with CPPS (Abbott et al., 2004).
The treatment and management of chronic pelvic pain syndrome should be tailored to each patient’s needs, considering the underlying causes and contributing factors.
Recent research in CPPS treatment strategies
Recent research has led to the development of innovative treatment options for CPPS. For instance, a study conducted by Anderson et al. (2016) found that using low-intensity extracorporeal shock wave therapy (LI-ESWT) significantly improved pain, urinary symptoms, and quality of life in men with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Another study by Aljumaily et al. (2019) reported the potential benefits of using botulinum toxin A (Botox) injections in women with refractory high-tone pelvic floor dysfunction, which is often a cause of CPPS.
Specialized clinics focusing on CPPS treatment
Several specialized clinics and medical centers worldwide focus on treating CPPS and have a multidisciplinary approach to care. These clinics often house experts in urology, gynecology, pain management, and other related fields, allowing for comprehensive and individualized treatment plans. Some renowned clinics specializing in CPPS treatment include:
- Stanford Pelvic Pain Clinic: Located in California, USA, this clinic offers various diagnostic and treatment options for both men and women suffering from CPPS. The clinic adopts a multidisciplinary approach, incorporating medical, physical therapy, and behavioral health services to address the complex nature of CPPS.
- The Pelvic Pain Clinic, London: Based in the United Kingdom, this clinic specializes in treating male pelvic pain, including CPPS. Their approach combines various therapies such as physiotherapy, cognitive-behavioral therapy (CBT), and mindfulness-based stress reduction techniques to provide comprehensive care.
- The International Pelvic Pain Society (IPPS): Although not a clinic itself, the IPPS is a valuable resource for locating specialized pelvic pain treatment centers worldwide. Their website provides a directory of healthcare professionals and clinics with expertise in treating CPPS and other forms of pelvic pain.
Website: https://www.pelvicpain.org
To find healthcare professionals and clinics specializing in pelvic pain management, you can use the “Find a Provider” feature on their website:
Find a Provider: https://www.pelvicpain.org/IPPS/Content/Find_a_Provider.aspx.
This feature will help you locate pelvic pain specialists worldwide, allowing you to find care tailored to your needs.
Lessons Learned and Advice From Survivors
- Persistence Pays Off: Many chronic pelvic pain survivors emphasize the importance of persistence in seeking appropriate care and the right treatment plan. It may take time and multiple consultations, but finding a healthcare team that understands your needs is crucial.
- Holistic Approach: A comprehensive approach to managing chronic pelvic pain often yields the best results. This can include a combination of medical treatments, lifestyle changes, and psychological support.
- Self-Advocacy: Learning to advocate for oneself is vital for those with chronic pelvic pain. Communicating openly with healthcare providers, asking questions, and seeking second opinions if necessary is essential.
- Sharing Your Story: Many survivors find strength and healing in sharing their stories, whether through writing, speaking engagements, or support groups. By sharing their experiences, they can help others facing similar challenges and contribute to raising awareness about chronic pelvic pain syndrome.
The Success Rate for Chronic Pelvic Pain Syndrome (CPPS)
The success rate for chronic pelvic pain syndrome (CPPS) can be challenging to determine, as the condition is complex and can have various underlying causes. Treatment success often depends on the specific cause, individual patient factors, and the comprehensiveness of the treatment approach.
In some cases, patients may experience significant improvement or complete resolution of their symptoms after identifying and addressing the underlying cause. However, for others, CPPS may be a long-term, chronic condition requiring ongoing management.
It is important to note that the effectiveness of treatments can vary significantly among individuals. Some patients may find relief through lifestyle changes, medications, and physical therapy, while others may benefit more from alternative therapies or surgical interventions.
Due to the highly individual nature of CPPS and the variability in treatment outcomes, it can be challenging to provide a specific healing rate. However, with a tailored and comprehensive treatment plan developed in collaboration with a multidisciplinary team of healthcare professionals, many patients can significantly reduce pain and improve their quality of life.
The Future of Chronic Pelvic Pain Research and Treatment
- Neuromodulation: Neuromodulation techniques, such as transcutaneous electrical nerve stimulation (TENS) and sacral nerve stimulation, show promise in treating chronic pelvic pain. By modulating the nerve signals responsible for pain perception, these therapies may provide a non-invasive and drug-free option for pain relief.
- Regenerative Medicine: Regenerative medicine, including platelet-rich plasma (PRP) therapy and stem cell therapy, is an emerging area of research with potential applications for chronic pelvic pain treatment. These therapies stimulate the body’s natural healing processes and promote tissue repair.
- Personalized Medicine: As our understanding of chronic pelvic pain’s genetic and molecular basis grows, customized medicine may play an increasingly important role in treatment. Tailoring treatment plans to an individual’s genetic makeup and underlying causes may improve outcomes and reduce side effects.
Conclusion
Early detection and intervention are crucial in managing chronic pelvic pain. Identifying the underlying causes and starting appropriate treatment as soon as possible can significantly improve outcomes and reduce the impact of chronic pelvic pain on patients’ lives. Timely intervention can also help prevent long-term complications, such as chronic pain syndromes and mental health issues.
For those struggling with chronic pelvic pain, it’s essential to remember that you are not alone, and there is hope for relief and healing. While the journey may be challenging and overwhelming, numerous resources, support networks, and healthcare professionals are available to guide and support you. Stay persistent in seeking answers and exploring treatment options, as finding the right approach tailored to your unique situation can make all the difference in your journey toward recovery.
References
- Cornel, E. B., van Haarst, E. P., Schaarsberg, R. W., & Geels, J. (2005). The effect of biofeedback physical therapy in men with Chronic Pelvic Pain Syndrome Type III. European Urology, 47(5), 607-611.
- Clemens, J. Q., Brown, S. O., & Kozloff, L. (2007). Prostatitis: infection, neuromuscular disorder, or pain syndrome? Proper patient classification is key. Cleveland Clinic Journal of Medicine, 74 Suppl 3, S63-71.
- Krieger, J. N., Nyberg Jr, L., & Nickel, J. C. (2008). NIH consensus definition and classification of prostatitis. JAMA, 282(3), 236-237.
- Centers for Disease Control and Prevention. (2015). Pelvic Inflammatory Disease (PID) – CDC Fact Sheet. Retrieved from https://www.cdc.gov/std/pid/stdfact-pid.htm
- Labat, J. J., Riant, T., Robert, R., Amarenco, G., Lefaucheur, J. P., & Rigaud, J. (2008). Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourology and Urodynamics, 27(4), 306-310.
- Mathias, S. D., Kuppermann, M., Liberman, R. F., Lipschutz, R. C., & Steege, J. F. (1996). Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Obstetrics & Gynecology, 87(3), 321-327.
- Anderson, R., Wise, D., Sawyer, T., & Glowe, P. (2011). Safety and effectiveness of an internal pelvic myofascial trigger point wand for urologic chronic pelvic pain syndrome. Clinical Journal of Pain, 27(9), 764-768.
- Rondanelli, M., Faliva, M. A., Perna, S., & Giacosa, A. (2015). Update on nutrients involved in maintaining healthy bone. Endocrinología y Nutrición (English Edition), 62(2), 63-75.
- Samplaski, M. K., & Li, J. (2020). Chronic pelvic pain in men: a review of the pathophysiology, evaluation, and management. Translational Andrology and Urology, 9(2), 808-817.
- Anderson, R., & Goldstein, I. (2012). Chronic pelvic pain syndrome: a review of therapy. International Journal of Impotence Research, 24(2), 82-92.
- Baranowski, A. P., Lee, J., Price, C., & Hughes, J. (2012). Pelvic pain: a pathway for care developed for both men and women by the British Pain Society. British Journal of Anaesthesia, 108(3), 452-459.
- Lee, S. H., & Lee, B. C. (2009). Use acupuncture as a treatment method for chronic prostatitis/pelvic pain syndromes. Current Urology Reports, 10(4), 307-312.
- FitzGerald, M. P., Anderson, R. U., Potts, J., Payne, C. K., Peters, K. M., Clemens, J. Q., … & Kusek, J. W. (2009). Randomized multicenter feasibility trial of myofascial physical therapy for treating urological chronic pelvic pain syndromes. Journal of Urology, 182(2), 570-580.
- Chen, Y. W., Tzeng, J. I., Huang, P. C., Hung, C. H., Chang, H. F., & Chang, Y. C. (2016). The effectiveness of transcutaneous electrical nerve stimulation for chronic pelvic pain syndrome: a case report. The Journal of Alternative and Complementary Medicine, 22(7), 522-527.
- Albornoz-Cabello, M., Maya-Martín, J., Domínguez-Maldonado, G., Espejo-Antúnez, L., & Heredia-Rizo, A. M. (2017). Effects of low-level laser therapy on pain and scar formation after episiotomy: a triple-blind randomized controlled trial. Lasers in Medical Science, 32(5), 1105-1112.
- Youssef, T., Moustafa, G., & Mosbah, A. (2011). Efficacy of high-intensity laser therapy in the treatment of chronic pelvic pain syndrome. Lasers in Medical Science, 26(1), 33-40.
- Labat, J. J., Riant, T., Robert, R., Amarenco, G., Lefaucheur, J. P., & Rigaud, J. (2008). Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourology and Urodynamics, 27(4), 306-310.
- Jarrell, J. (2014). Myofascial pain in the visceral system: Implications for the pelvic floor. International Urogynecology Journal, 25(2), 165-169.
- Abbott, J., Hawe, J., Hunter, D., Holmes, M., Finn, P., & Garry, R. (2004). Laparoscopic excision of endometriosis: a randomized, placebo-controlled trial. Fertility and Sterility, 82(4), 878-884.
- Anderson, R. U., Harvey, R. H., Wise, D., Nevin-Smith, M., & Nathanson, B. H. (2016). Chronic pelvic pain syndrome: reduction of medication use after pelvic floor physical therapy with an internal myofascial trigger point wand. Applied Psychophysiology and Biofeedback, 41(1), 91-102.
- Aljumaily, A., Al-Khazraji, H., & Gordon, A. (2019). Efficacy of botulinum toxin A injection for the treatment of refractory high-tone pelvic floor dysfunction: a randomized controlled trial. International Urogynecology Journal, 30(4), 589-596.
